MSD has announced the UK launch of Zinplava® (bezlotoxumab) – a new therapy for the prevention of recurrence of Clostridium difficile infection (CDI) in adults at high risk for recurrence of CDI.1
Bezlotoxumab is administered as a single, one-off, one-hour intravenous infusion alongside standard-of-care (SoC) antibiotic therapy for the treatment of CDI.1
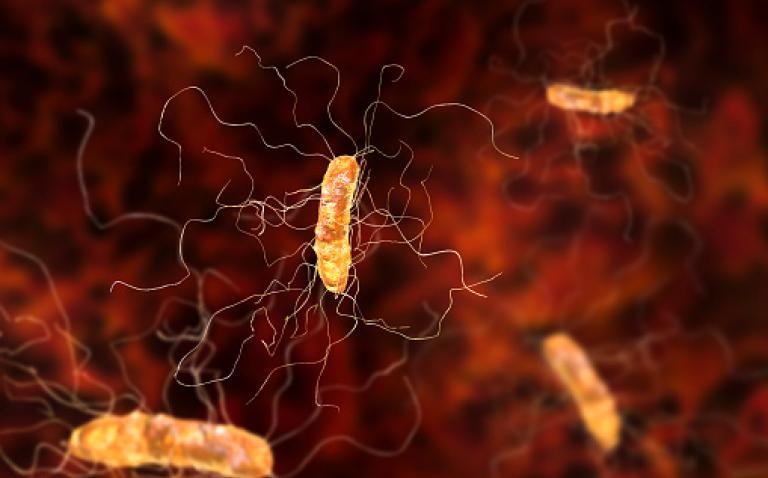
Clostridium difficile (C. difficile) is a bacterium that colonises the bowel and lives in the colon without causing disease in up to 3% of adults.2 C. difficile produces toxins, (principally toxins A and B) that can lead to damage of the lining of the colon, causing a range of symptoms from mild diarrhoea to perforation of the colon, sepsis and death.2
In the financial year 2016/17, there were 12,840 cases of CDI reported in England.3 Patients who develop CDI are usually given an antibiotic to treat the infection, but CDI can often come back within weeks or months. For hospitalised patients, the rate of recurrence is around 20% after the first episode and 45–60% after a second episode of CDI.2 The mortality rate of CDI infection can be up to 25% in frail, elderly people in hospitals.2 Repeat episodes are associated with an increased number of hospitalisations and therefore higher costs.4
Antibiotics are used to treat CDI, but they also may further disrupt the gut microbiota, making some patients vulnerable to CDI recurrence.5
Mark Wilcox, Professor of Medical Microbiology at the University of Leeds, commented: “Bezlotoxumab is the first therapy for CDI that targets the toxin that causes this disease. Notably, bezlotoxumab reduces the risk of the recurrence of CDI for at least 3 months, compared with standard of care antibiotic therapy. This is welcome addition to our limited options to reduce the considerable morbidity and mortality associated with CDI.”
Bezlotoxumab is a human monoclonal antitoxin antibody that binds with high affinity to C. difficile toxin B and neutralizes its activity. Bezlotoxumab prevents CDI recurrence by providing passive immunity against toxin B produced by the outgrowth of persistent or newly-acquired C. difficile spores.1 Bezlotoxumab is not a treatment for CDI and has no effect on the current CDI episode. The experience with bezlotoxumab in patients is also limited to a single CDI episode and single administration.1
“The launch of bezlotoxumab in the UK continues MSD’s longstanding tradition of bringing forward novel therapies to address serious infectious diseases, and we are proud to add this important treatment to our existing portfolio of anti-infective medicines,” said Dr Mike England, MSD’s Interim Medical Director. “Antimicrobial resistance is a key national issue and we hope with bezlotoxumab to not only help achieve a reduction in the number of recurrent episodes of CDI but also a reduction in the amount of antibiotic prescriptions that would otherwise be needed to treat these recurrent episodes.”
The efficacy of bezlotoxumab was investigated in a landmark clinical trial programme including two large phase III studies (MODIFY I and MODIFY II) in which patients received bezlotoxumab plus SoC antibacterial therapy for CDI (metronidazole, vancomycin or fidaxomicin) vs. SoC alone. Results from these studies were published in the New England Journal of Medicine.6
Patients enrolled in these randomised, double-blind, placebo-controlled, multicentre, Phase III studies were 18 years of age or older and had a confirmed diagnosis of CDI. Patients were randomized 1:1:1 to receive bezlotoxumab, bezlotoxumab plus actoxumab, or placebo, in addition to standard of care antibacterial therapy. In MODIFY I, patients were also be randomised to actoxumab, but this arm was discontinued after a planned interim analysis. Actoxumab was found not efficacious when given alone and provided no additional benefit when given with bezlotoxumab. These observations are consistent with evidence indicating that toxin B is the main determinant of virulence in recurrent CDI in humans.
In both trials, the rate of recurrent CDI was significantly lower with bezlotoxumab (plus SoC) than with placebo (plus SoC) (MODIFY I: 17% [67 of 386] vs. 28% [109 of 395]; adjusted difference, -10.1 percentage points; 95% confidence interval [CI], -15.9 to -4.3; P<0.001; MODIFY II: 16% [62 of 395] vs. 26% [97 of 378]; adjusted difference, -9.9 percentage points; 95% CI, -15.5 to -4.3; P<0.001) and was significantly lower with actoxumab plus bezlotoxumab (plus SoC) than with placebo (plus SoC) (MODIFY I: 16% [61 of 383] vs. 28% [109 of 395]; adjusted difference, -11.6 percentage points; 95% CI, -17.4 to ?5.9; P<0.001; MODIFY II: 15% [58 of 390] vs. 26% [97 of 378]; adjusted difference, -10.7 percentage points; 95% CI, ?16.4 to -5.1; P<0.001).6
Bezlotoxumab demonstrated reduced rates of recurrence in pre-specified subgroups of patients at high risk for CDI recurrence, including patients 65 years of age and older, those with a history of one or more episodes of CDI in the past 6 months, immunocompromised patients and patients with severe CDI.
In the MODIFY I and MODIFY II studies, the most common adverse reactions following treatment with bezlotoxumab (reported in ≥4% of patients within the first 4 weeks of infusion) were nausea, diarrhoea, pyrexia (fever) and headache. These adverse reactions were reported at a similar frequency in placebo treated patients compared with bezlotoxumab treated patients.1
References
- Summary of Product Characteristics (SPC) Available at: https://www.medicines.org.uk/emc/medicine/33452
- NICE, Preventing recurrence of Clostridium difficile infection: bezlotoxumab (2017), available at: https://www.nice.org.uk/advice/es13/chapter/Introduction-and-current-guidance
- Public Health England, C. difficile infections: quarterly counts by acute trust and CCG, and financial year counts and rates by acute trust and CCG, up to financial year 2016 to 2017, available at: https://www.gov.uk/government/statistics/clostridium-difficile-infection-annual-data
- Aitken SL, Joseph TB, Shah DN, Lasco TM, Palmer HR, et al. (2014) Healthcare Resource Utilization for Recurrent Clostridium difficile Infection in a Large University Hospital in Houston, Texas. PLoS ONE 9(7): e102848. doi:10.1371/journal.pone.0102848
- Seekatz. A, M, Clostridium Difficile and the gut microbiota, J Clin Invest. 2014;124(10):4182–4189. doi:10.1172/JCI72336.
- Wilcox. M. H. Bezlotoxumab for Prevention of Recurrent Clostridium difficile Infection (2017), New England Journal of Medicine 376;4