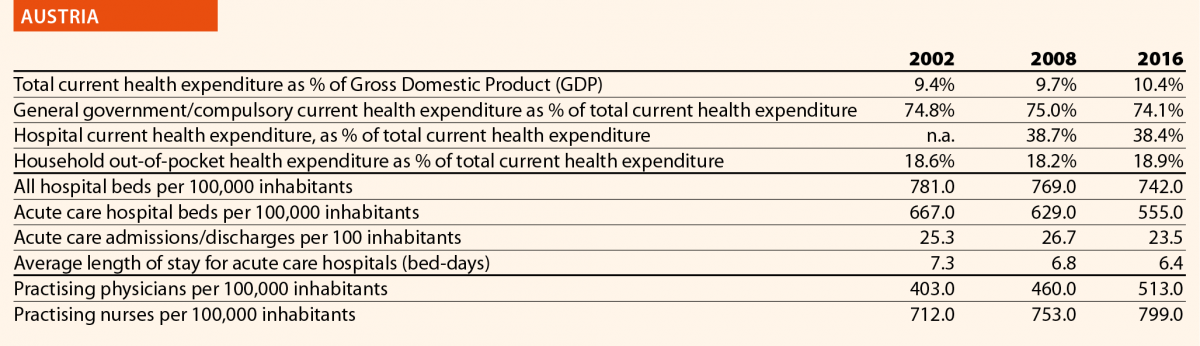
Austria

Mr Nikolaus Koller
HOPE Governor

Mrs Ulrike Schermann-Richter
HOPE Liaison Officer, Federal Ministry of Labour, Social Affairs, Health and Consumer Protection
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
Due to the federalist structure of the state and the self-governed system of compulsory insurance, the Austrian healthcare system is characterised by a fragmentation of responsibilities for regulating, planning, financing and providing healthcare between the different legislative as well as administrative levels (federal and regional governments) and the social insurance funds.
The rather complex blend of different decision-making structures favours frictional losses and inefficiency. However, streamlining the historically grown constitutional competences was never feasible.
The growing pressure on health systems during, and in the aftermath of the economic crisis, gave impetus for a reform that aimed to overcome the traditional fragmentation and to improve coordination and policy coherence. In 2013, thus, a target-based health governance system for the joint management of the structure, organisation and financing of the Austrian healthcare system was established. The system is based on domestic state treaties, which are concluded for a limited period of time (4–5 years) between the federal and the regional governments with the involvement of the social insurance institutions, while leaving the constitutional division of powers and responsibilities unchanged.
In 2017, the second Federal Target-Based Governance Agreement was signed. It sets four strategic goals that are further specified in eleven objectives, concrete indicators and targets and almost 80 measures to be taken at federal and/or regional level over a period of five years. The strategic goals are:
- Strengthening ambulatory care while reducing overuse of the inpatient sector and optimising allocation of resources;
- Ensuring satisfaction of the population by optimising care and treatment processes;
- Strengthening health promotion and prevention;
- Ensuring financial sustainability of public health expenditure.
In December 2018, a reduction of the number of social insurances funds was decided by the Parliament inter alia by merging the nine regional health insurance funds into a single one covering almost the 80 % of the population. Savings in administration and efficiency gains are expected.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
A significant reform activity was the development of a new approach to the provision of primary healthcare, which is traditionally provided by individual general practitioners working alone in private practices, contracted to one or more social insurance funds. In 2017, the Primary Health Act was adopted, laying down uniform requirements for the new primary care across Austria. In the same year, the establishment of a total of 75 multi-professional and interdisciplinary primary care centres and networks, respectively, by the end of 2021 was agreed. The new primary care units are to be achieved by attracting existing GPs and other health professionals working together in teams, thus being able to provide more comprehensive services and more opening hours for the patients while, coincidently, the working time is better distributed between the team members, favouring a better work–life balance.
A few primary care units are already in operation and are well accepted by the patients. The medical staff also seems to be satisfied. In order to promote the new concept, appropriate contractual agreements are under negotiation and start-up programmes are being developed. Strengthening primary care is crucial as the Austrian health system has still a strong focus on hospital (inpatient) care.
The introduction of the Electronic Health Record (ELGA), together with its e-medication and e-report applications, is making good progress. Since the end of 2015, ELGA is being rolled-out in stages, starting with public hospitals. Between March 2018 and September 2019, ELGA and e-Medication are being made available step by step to doctors in private practices, group practices, pharmacies and outpatient clinics. The aim of ELGA is to reduce organisational barriers, improve coordination and strengthen patients’ rights.
Whether the recent reform of the organisational structure of the health insurance funds will affect the healthcare system will only become apparent in the coming years.
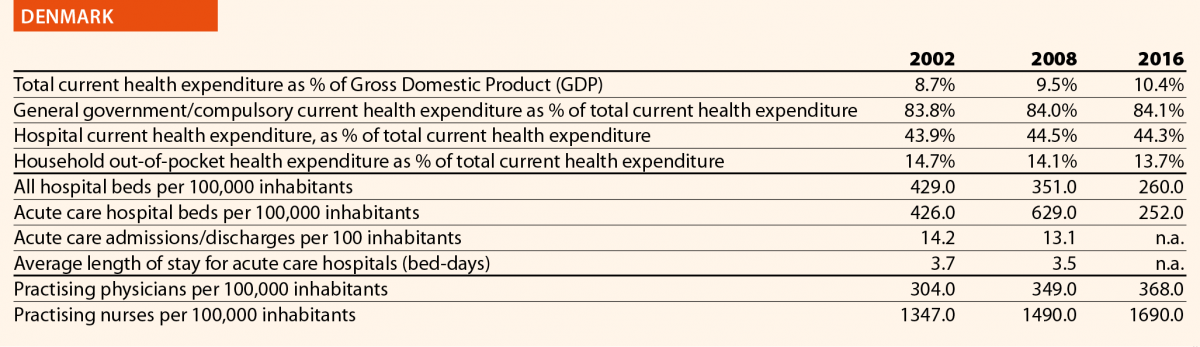
Denmark

Mrs Eva M Weinreich-Jensen
HOPE President, Danish Regions
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
A major reform of the Danish healthcare sector took place in 2007. Following the reform, the number of hospitals was heavily reduced and concentrated, and the specialised hospital services were centralised. Whatever has been done after 2007 has been an attempt to add to, and to adjust, the 2007 reform.
One example is the National Strategy for Personalised Medicine 2017–2020, involving a national infrastructure working on both treatment and research. Moreover, regional data support centres will be established, providing researchers, clinicians and health personnel with reliable data.1
Another example is the National Digital Health Strategy 2018–2022, based on 25 specific initiatives empowering patients by giving them a complete overview of their digital health data and by offering them a digital copy of their health records.2
A third example is the National Strategy for Cyber and Information Safety in the Healthcare Sector 2019–2022, which aims to make the digital system in health secure and trustworthy, given the amount of patient data handled.
At the moment, the Danish Region is looking at a national wish to reform the outpatient system and to make patients’ paths easier and more flexible while ensuring a better coordination of care. The focus shall be also on how to face the demographic challenges by changing the structural mind-set. This may come in the form of defining health communities around 21 acute hospitals; an increased cooperation between general practitioners and the hospitals and an overall strengthening of the pre-hospital effort and the acute functions. The overall trend is a change from focus on treatment activity and volume, to prevention and quality treatment (outcomes). The basic goal is to give patients a better service by increasing the possibility to diagnose and treat them at home or in primary settings, while, at the same time, reducing the burden to the hospitals.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
Adjusting the incentives of the system is an ongoing process, especially when it comes of adapting to a reform. The focus is now on changing a silo-based approach to treatment, adopting a more holistic view empowering patients; improving patient pathways; creating a strategy for digital development; investing in personalised medicine; providing transparency to patients for what concerns their health data; and encouraging initiatives on cybersecurity and the use of new technology. Health workforce needs to be supported and trained on how to face these changes and challenges.
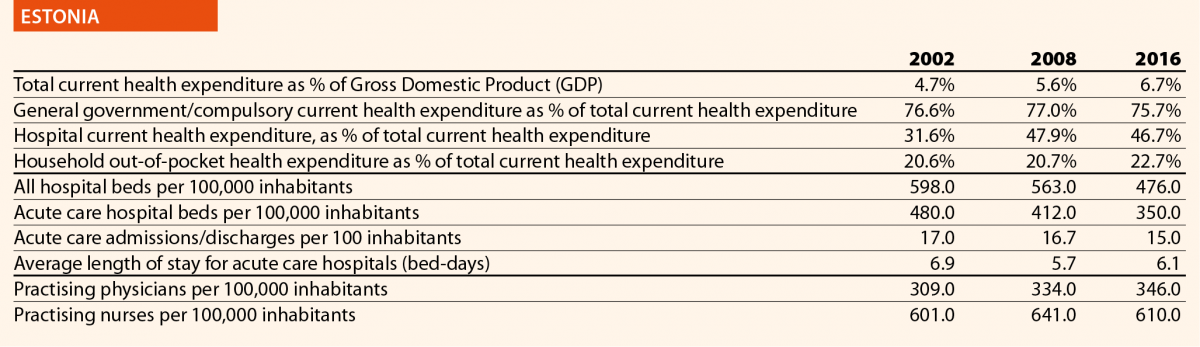
Estonia

Mr Urmas Sule
HOPE Vice-President, Estonian Hospitals Association
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
In 2017, the Estonian government made a historic and long-awaited decision about healthcare system financing. The Estonian healthcare system is mainly publicly funded through solidarity-based mandatory health insurance contributions in the form of an earmarked social payroll tax (13% of wages). The health insurance system covers about 94% of the population.
Contributions are related to employment, but the share of non-contributing individuals covered by the Health Insurance Fund (for example, children and pensioners) represents more than half of the insured. Health Insurance Fund revenue base has been dependant on the amount of working people paying social tax, but not unlike other countries, Estonia is also facing the challenges of an ageing population.
So finally, in 2017, in close cooperation with the healthcare social partners, the Estonian government promoted the initiative of expanding the revenue base of the health system, which has been a longstanding challenge. The government decided to broaden the Health Insurance Funds revenue base by gradually increasing a state contribution into the Health Insurance Fund on behalf of pensioners, starting from 2018. By 2022, this contribution should reach 13% of average pensions, which is the same rate as the current earmarked social health insurance contribution from payroll tax. This will not solve all problems, but it is definitely a step in the right direction. Thanks to this decision it was possible to renew the nationwide collective agreement in the health sector.
This decision impacts also on other services previously covered by the state budget. For example, emergency care (including for non-insured people), ambulance care and IVF are, or will, be under the responsibility of the Health Insurance Fund. The aim of the change was to make the healthcare system more efficient by strengthening the purchasing role of the Health Insurance Fund and making it responsible for financing health services for the whole population and not only for the insured.
Estonia is continuously focusing on developing e-health solutions to improve the quality and availability of healthcare services. In 2019, Estonia will launch a statewide digital project to increase health service provision transparency and availability.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
The previously mentioned reform will not lead to a significant increase in total public health expenditure, but it will consolidate previously fragmented service funding under the Health Insurance Fund. Consequently, the Health Insurance Fund budget will increase significantly in the following years, but at the same time it will also have more responsibilities. However, the funding of the health system will be more logic. In summary, this reform is a good example of Estonia adapting to new situations and challenges, finding innovative solutions, but there is still work to be done in achieving a more sustainable financing system of healthcare.
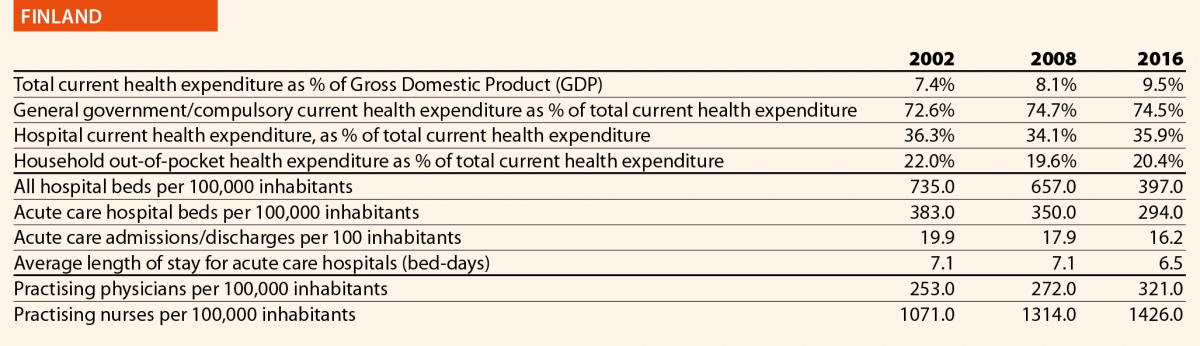
Finland

Mrs Hannele Häkkinen
HOPE Governor, The Association of Finnish Local and Regional Authorities
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
One of the initiatives implemented in recent years was the division of healthcare services provided between secondary hospitals and centralised hospitals. In particular, centralised hospitals are now in charge of demanding and providing rare treatments and diagnostics, for example, surgical operations including hip and knee replacement, as well as childbirths. The five university hospitals offer the most demanding treatment. The goal is to guarantee equal access to services, sufficient skills and knowledge to health professionals, patient safety as well as to curb the cost growth.
A second initiative is the introduction of joint emergency care units (primary and secondary care) in central hospitals and the division of work between nurses and doctors in primary care and emergency care in hospitals.
Finally, the Health and Social Services Reform is ongoing. The goal is to put primary care, secondary care and social care under one umbrella. At the moment the municipalities are responsible for organising health and social services. This responsibility will be transferred to 18 new counties on 1 January 2021. The law proposal is in Parliament but it is uncertain as to whether it will be approved because there will be parliamentary elections in April 2019.3
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
The goals of the centralisation of the most demanding and rare treatment to fewer hospitals are better cost-efficiency, better quality of care and treatment and better patient safety.
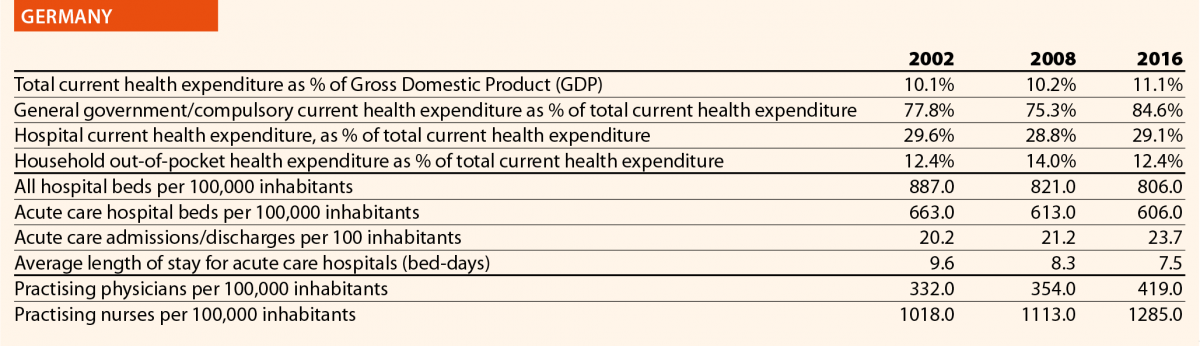
Germany

Mr George Baum
HOPE Governor, German Hospital Federation
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
In the last 5 years, political priorities have focussed on the continuous development of quality assurance and of the reimbursement systems for healthcare providers. Additionally, a great importance has been given to measures to face the challenge of health workforce shortage.
In 2015, the so-called Hospital Structures Act (Krankenhausstruktur-Gesetz) enforced quality assurance in hospitals; improved financing of nurses and strengthened patient safety as regard nosocomial infections by fostering a hygiene support programme. This act entered into force on 1 January 2016 and included the following key aspects:
- Establishing a job promotion programme for nurses for the years 2016–2018 with a total volume of 660 million Euros;
- Transforming a former extra-fee to safeguard structures for healthcare provision (Versorgungszuschlag) into an extra-fee for care (Pflegezuschlag) with an overall volume of 500 million Euros;
- Introducing binding quality indicators for hospital planning;
- Developing further initiatives on quality such as patient friendly quality reports, quality contracts as well as quality-associated extra-fees and deductions;
- Establishing funds for the improvement of healthcare-structures with a volume of 500 million Euros;
- Definition of minimum standards for hospitals for the provision of emergency care.
The training of nurses has been subject of reform with the 2015 Nursing Professions Reform Act (Pflegeberufereformgesetz). Training for nurses, paediatric nurses and long-term care nurses have been merged into a unique programme.
With a law on the continuous development of provision and reimbursement of psychiatric and psychosomatic care in the year 2016, a services-oriented financing for hospitals has been introduced. Transparency has been enhanced and a better coordination of inpatient and ambulant services enabled.
In May 2018 the most important hospital act in the running legislative period for hospitals has been forecasted. With the Care Personnel Strengthening Act (Pflegepersonalstärkungsgesetz), the general status of nursing and long-term care shall be improved. It is focussed on the full reimbursement of labour costs for care personnel and its extraction of the DRG-system starting with the year 2020. Additionally, partners of the self-governance system (health insurances and services providers) have been mandated to extend the already existing minimum levels for care personnel to further departments in the hospitals. This law came into force at 1 January 2019.
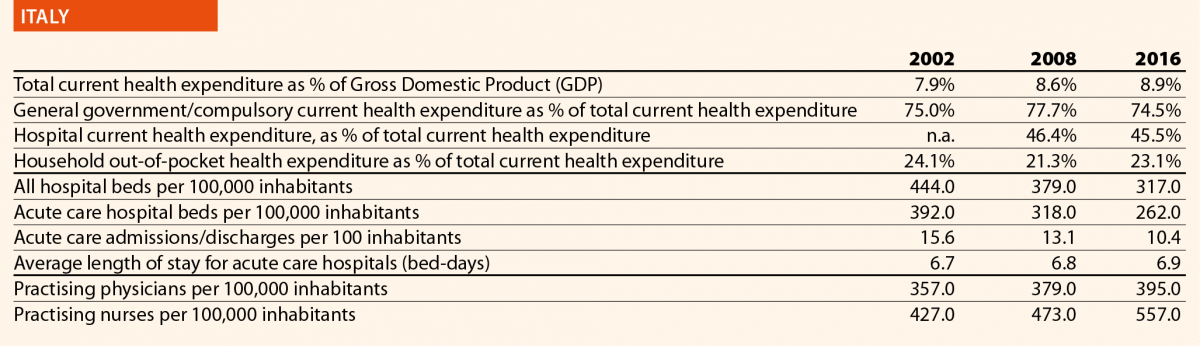
Italy

Mr Domenico Mantoan
HOPE Governor, Veneto Region
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
In the past 5 years, as regards the hospitals, the most important law is the National Decree n.70/2015. It states the new hospitals standards (structural, technological, organisational and clinical) that have to be applied in each Italian Region. The decree states that each Italian Region has to create a network of acute hospitals, based on three hierarchical levels: basic hospitals (serving a population of 80,000 – 150,000 inhabitants); first level hospitals (serving a population of 150,000–300,000 inhabitants); second level hospitals (serving a population of 600,000–1,200,000 inhabitants). It states, also, the criteria for the number and type of clinical departments. For example, cardio-surgery departments have to serve a population between 600,000 and 1,200,000 inhabitants. The decree states also the operative standards; for example, each breast surgery department has to treat at least 150 cancer cases per year.
As regards general aspects of healthcare, a National law was approved in January 2017, regarding the new so-called essential levels of assistance (LEA – Livelli Essenziali di Assistenza). The LEA represents the minimum levels of health services that have to be provided by the Italian National Health System (NHS) through public national funding. Some LEA must be provided for free (that is, acute hospital inpatient services) whereas others need to be covered through a co-payment from the patient. New LEA legislations have come after a long period without any national update. In fact, the last (and first) national LEA legislation was in 2001.
As regards the healthcare reform, an innovative regional reform commenced in Veneto in 2016. It is based on two main topics: the reduction of the number of Health and Social Local Trusts (HSLTs) and the creation of an innovative Trust, called Zero Trust (Azienda Zero), which absorbed some functions – mainly administrative – that were previously performed by other Trusts or regional offices. The Zero Trust does not provide any clinical services. It was conceived with the aim of increasing efficiency and productivity through a more effective use of resources, following a unified approach.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
Regarding national hospitals standards, each region had to reorganise its inpatient settings by reducing the number of acute hospital beds. The organisational impact was important because outpatient care and home care were strengthened. Country hospitals were implemented too. Hospitals teams are encouraged to work in network. Clinical networks (oncological, cardiologic and emergency networks) were created. Some departments were closed such as the surgery departments being under standard in terms of number of interventions.
As regards new LEA legislation, it has introduced some free vaccinations that previously were not covered, namely vaccinations against papilloma virus, meningococcus and pneumococcus. The introduction of new screening tests in newborns, such as tests for congenital deafness and cataract, had an important impact. For disabled individuals, new information technology was introduced. For example, eye gaze control systems and speech generating devices are covered for severe stages of paralysis (such as in severe amyotrophic lateral sclerosis). At the same time, the new LEA restricted the coverage of some types of treatment, particularly dental care.
Veneto Region went through a reform reducing the number of Trusts from 21 to nine. The impact of such reform was important because this resulted in a new distribution of competences. The Zero Trust centralised all the administrative functions such as nursing recruitment, large procurement, regional education and health technology assessment. The centralisation of ICT services offers a new important challenge for storing and managing health and organisational information in a unique digital archive.
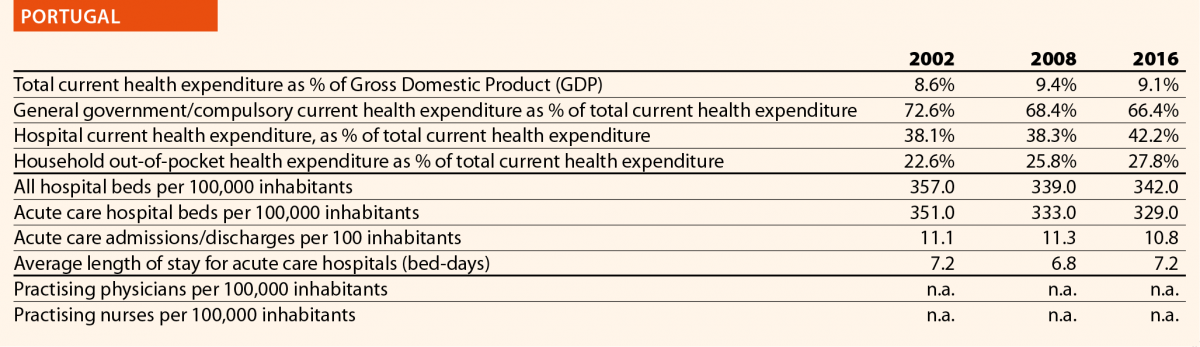
Portugal

Mr Carlos Pereira Alves
HOPE Governor, Portuguese Association for Hospital Development
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
Primary healthcare reform4
In recent years, the Primary Healthcare Network has been strengthened and expanded, through the deepening of the Primary Health Unit’s model and performance, with the objective of increasing the NHS response and assigning a family health team to all residents.
Integrated responsibility centres
In 2018, the model of Integrated Responsibility Centres (CRIs) that are organic intermediate management structures, dependent on the NHS public entities boards of directors was defined.5 The CRIs have functional autonomy and establish an economic and financial assistance commitment, following the presentation of an action plan that defines the healthcare programme for a period of three years. The CRIs are created to ensure the development of best clinical practices focused on the users’ needs; foster clinical governance processes and therefore care quality improvement; increase the accessibility and timely response of the NHS to citizens; mobilise the installed capacity in the NHS public network; promote the autonomy and involvement of professionals holding managerial responsibilities; and increase NHS professionals’ productivity and satisfaction levels, linking the institutional and financial incentives allocation to the performance effectively achieved.6
Affordable and quality palliative care7
The Strategy for the Development of Palliative Care resulted in a National Network of Palliative Care, integrated in the NHS and implemented at all levels of healthcare.
Digital transformation (E-Health)
In 2017, the National Strategy for Health Information Ecosystem 2020 was approved,8 which aims to increase citizens’ interaction with health technology. To this end, it provides the availability of multiple digital service platforms that allow information access and sharing, but also the simplification and informatisation of registries and processes in the NHS till 2020 such as E-Prescription, Electronic health record, Portal SNS9 and mobile applications (MySNS,10 MySNS TEMPOS,11 MySNS CARTEIRA12).
Clinical Academic Centres and University Hospitals
In 2018, Clinical Academic Centres were created and pilot projects of University Hospitals were established.13 Clinical academic centres are consortiums and associations of healthcare units (for example, hospitals), higher education institutions (for example, universities) and/or research institutions (public or private). These centers are dedicated to the promotion of integrated healthcare, teaching, clinical research and translation. With the pilot projects of university hospitals, some established university hospital centres were reorganised to improve their working processes and functions.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
The reinforcement and expansion of the Primary Healthcare Network significantly improved primary healthcare, in terms of accessibility and quality. On one hand, this is visible by the increase in the number of Portuguese with family doctor (93 % in 2017); and on the other hand, by the number of medical appointments, which is over 30 million per year. In January 2018, the highest number of physicians, nurses and diagnostic and therapeutic technicians, working in the NHS, in the last ten years was registered.
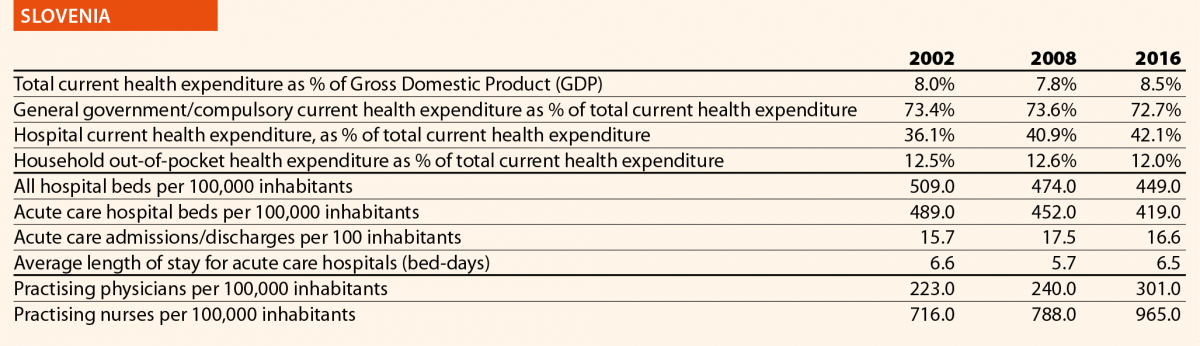
Slovenia

Mr Simon Vrhunec
HOPE Governor, Association of Health Institutions of Slovenia
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
Slovenia is still among the countries in the EU that spend less than average on healthcare. If EU average health expenditure is 9.6% of GDP in 2017 (Health at a Glance: Europe 2018), in Slovenia it was only 8.0% of GDP the same year. In addition to the lack of financing resources Slovenia is facing also a lack of practicing doctors. In Slovenia there are 3 practising doctors per 1000 population while the EU average is 3.6 (Health at a Glance: Europe 2018). Only with practising nurses is the situation slightly better, because this figure is above the EU average in Slovenia.
A lack of resources in the Slovenian healthcare system results in long waiting times for specialist outpatient care. Some waiting times exceed a year and 40% of those who are waiting for a specialist outpatient service are waiting more than it is considered acceptable. Despite those facts, in politics there is still a very strong opinion that the main cause for long waiting times is corruption and not lack of resources, which is why no serious reform was implemented in the last five years. The only change of health law was to prevent (forbid) doctors to work for different employers and to decrease the validity of concessions from an indefinite term to 15 years.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
Because the healthcare legislation was changed only one and a half year ago and the providers are still inside the three-year period to adopt the changes, there are no elements of the impact present. But the expectation is that restrictions for doctors to work on different locations will result in increasing waiting times and not the opposite.
Spain

Mrs Sara Pupato Ferrari
HOPE Governor, Ministry of Health, Social Services and Equality
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
Central procurement in the National Health System
On December 2001, the transfer of managerial processes regarding the National Healthcare System concluded with the decentralisation of decision-making centres to the 17 Autonomous Communities (CCAAs), the National Healthcare System itself and the National Health Management Institute (INGESA).
The decentralisation brought a very fragmented, opaque and, in some way, inefficient procurement market policies that required a rationalisation of the procurement system.
A Central Purchasing Unit dealing with all the National Healthcare System procurement procedures was considered a useful alternative for that, with the aim of:
- Ensuring equity and cohesion through the implementation of new quality standards and technical criteria that every product should comply with;
- Promoting transparent procurement policies and easing market competition;
- Gaining efficiency and increasing budget savings.
During 2014, pharmaceutical products restricted to hospital use were declared as central procurement system products and INGESA was entrusted to develop the acquisition procedures. From 2015, most CCAAs (the exceptions being the Basque Country, Catalonia, Andalusia and the Canary Islands) have supported and participated in the emerging acquisition system replacing old punctual acquisition agreements and a Central Procurement Agency was implanted in INGESA aiming to get the support of the CCAAs. Despite the achievements, centralised procurement raised several issues and was partially used.
Strategic National Plan against Hepatitis C
Four years ago, the Strategic National Plan against Hepatitis C was established, and major achievements have occurred since then. An update of the Plan Against Hepatitis C has been approved by the National Health System Interterritorial Health Council and now new challenges have to be embraced to make this policy effective. The collaborative diagnoses and treatment of social groups that do not know whether or not they are infected also has to be achieved.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
Central procurement in National Health System. Recently a centralised acquisitions digital tool has been introduced by the Ministry of Health, Consumers Affairs and Welfare. The tool is based on an Information Platform Collaborative Web that allows access to the participating agents to all the information related to centralised acquisition initiatives in an anonymous way.
It also incorporates a virtual forum so different agents can share problems and good practices on line easing collaboration in some issues such as catalogue definition, contract files development and criteria. Having elaborated a centralised acquisition products catalogue integrated in the platform, nearly 25,000 items structurally and hierarchically classified have been included. The catalogue structure will allow incorporation of medical services in the future. With this tool, a budget saving close to 500 Million Euros is anticipated in the coming years.
Hepatitis C strategy
Access to effective treatment could be considered fulfilled and to date, more than 117,000 patients can be considered cured in Spain.

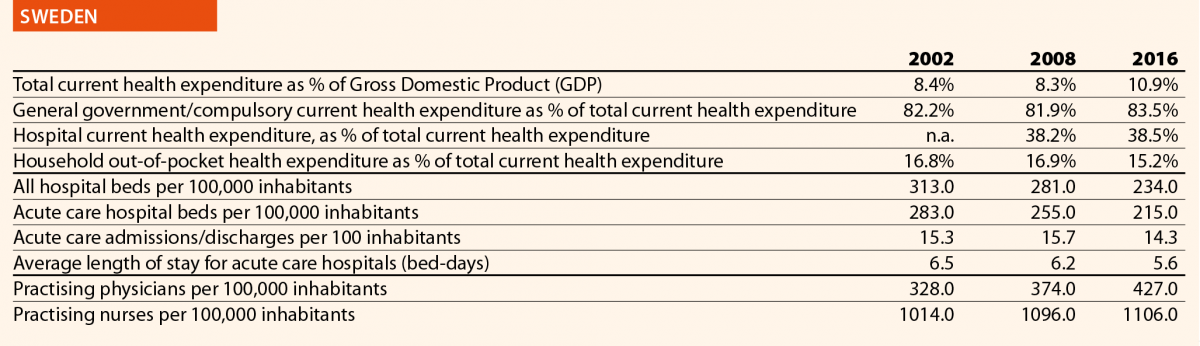
Sweden

Mr Erik Svanfeldt
HOPE Governor, Swedish Association of Local Authorities and Regions (SALAR)
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
In 2015, a new Patient Act came into force, which increased the opportunities for patients to choose healthcare provider – public or private – in outpatient care. In Sweden, the regions are responsible for the financing and provision of healthcare, and there are sometimes differences concerning what services they offer. In the past, the patients had limited possibilities to seek planned healthcare outside their home region, but since 2015 patients may also seek outpatient treatments in other parts of Sweden that are not included in their home region health basket.
In July 2018, a new decision-making process for national highly specialised healthcare was established. Sweden already had a system for coordination of very highly specialised healthcare, giving a national committee the right to concentrate certain services to just one or two hospitals in the entire country. But in order to improve quality and equality in healthcare, the National Board of Health and Welfare can now decide to concentrate specific healthcare services to up to five hospitals.
In parallel, work on level structuring and standardised care processes in cancer care is ongoing. Proposals have also been submitted on how to make the Swedish healthcare more efficient by improving community care. In 2018, a new law on cooperation at discharge from inpatient healthcare was implemented. The aim is to improve the care for those people who need both outpatient healthcare and the assistance of the municipal social services.
The regions have, one by one, enabled patients to access their own patient records online.
In 2013, a new legislation on health and medical care to foreigners who stay in Sweden without necessary permissions as implemented. The regions have to offer these people health and dental care who urgently require it.
The Swedish Parliament has recently decided to reform the training of doctors in 2020.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
The new Patient Act, introduced in 2015, has had at least two noticeable effects. First of all, the new legislation, together with the EU Patient Mobility Directive from 2011, has widened Swedish patients’ access to European healthcare. Since 2015, the most generous region sets the bar concerning the patient’s rights to care and reimbursement. If one region offers a specific treatment, all Swedish patients have the right to receive this care on equal conditions also in another EU/EES member state.
Similarly, the legislation has allowed patients to make medical appointments and have video consultations via smartphone, personal computer or tablet across regional borders. A healthcare provider offering digital services can now establish in just one region and serve the entire country. In Sweden, each region decides on their own patient fees, mechanisms for paying the providers and remunerations, but because of these new cross-border digital services, there was a need for SALAR to adopt recommendations concerning the level of remuneration to the providers and uniform patient fees.
Concerning level structuring and standardised care processes in cancer care, the Swedish Government and SALAR in 2015–2018 implemented a national effort to shorten waiting times and reduce regional differences in cancer care by introducing cancer patient pathways. These pathways aim to shorten the time between a well-founded suspicion of cancer and the start of the first treatment. Another goal was to create a more equal and predictable care with increased quality and improved patient experience.
This national effort is monitored by following the waiting times and patient reported experience measures (PREMs). The measurements show high overall patient satisfaction with the cancer care and the national effort has also led to better communication within and between hospitals and regions. But so far, it has been difficult to influence waiting times, partly due to problems of lack of staff.
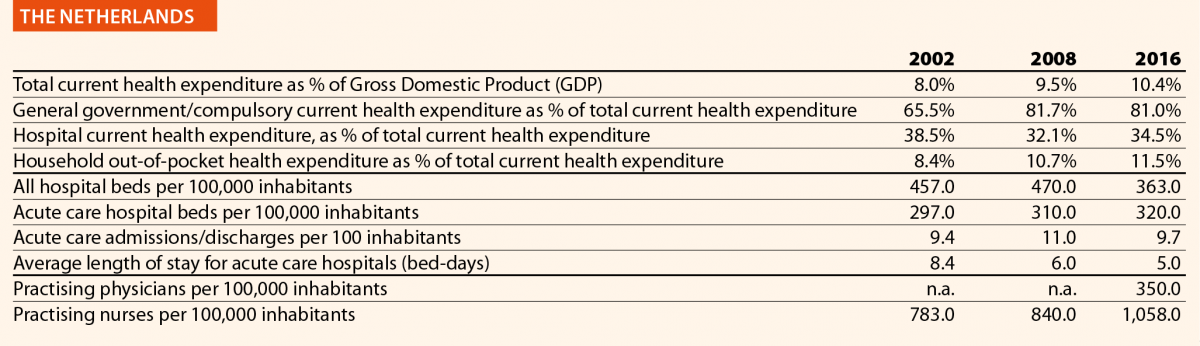
The Netherlands

Mr Sander Gerritsen
HOPE Governor, Dutch Hospital Association
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
A significant healthcare reform took place in 2006. It replaced the division between public and private insurance with one universal social health insurance. It also introduced managed competition as a driving mechanism. Although this reform was initiated over a decade ago and the principles of the new system have since then remained intact, its stepwise implementation continues to bring changes in the healthcare system.
Since 2015, there is one integrated reimbursement rate for hospital treatments. Until then costs were claimed partially by doctors and partially by hospitals. In the new system hospitals claim the entire costs for the treatment. It is up to them to distribute the money. This has led to new forms of cooperation between the doctors and the hospital management.
In 2015, the General Act on Exceptional Medical Expenses, which related to long-term care and nursing, was dismantled. The costs were running out of control and the government decided to act. Most of the tasks were decentralised and became the responsibility of the municipalities.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
The first challenge concerns the monitoring of costs when there is a market-based system (production driven) while the demand for care is constantly growing.
The new financial structure has had its challenges. Doctors have formed separate medical specialist companies within the hospital structure. Hospitals have been struggling for longer to find the best ways to incorporate such companies within the hospitals. Nonetheless the Dutch Health Authority (NZa) concluded in 2018 that this reform has had positive effects on this cooperation (professionalisation, efficiency, shared responsibility).
Decentralisation of tasks does not simply lead to a reduction of costs. When you decentralise the long-term care without transferring enough funds, in the long run it might even have an adverse effect. One example is the closing of nursing homes, which led to a rise in the number of vulnerable elderly patients in hospitals.
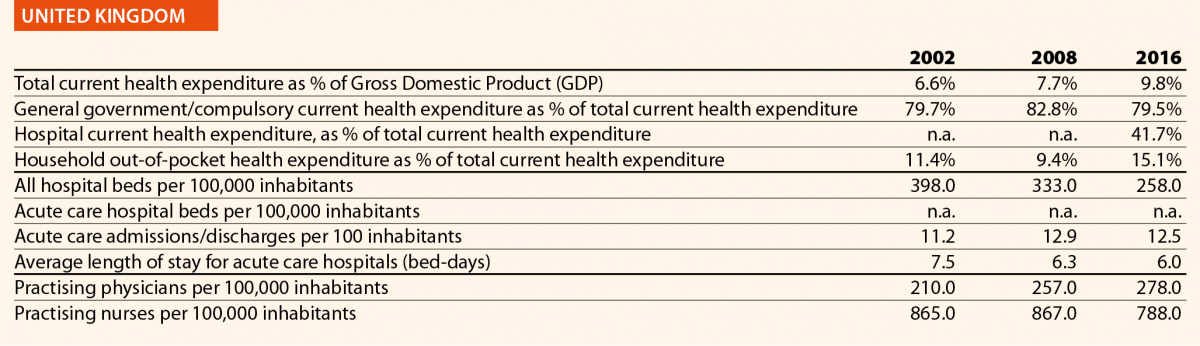
United Kingdom

Mr Niall Dickson
HOPE Governor, NHS Confederation
Could you describe the last hospital and/or healthcare reforms implemented in your country in the past 5 years?
NHS Long-Term Plan
In January 2019, NHS England published the Long-Term Plan, setting out a strategy for the health service for the next ten years. It is a wide ranging and ambitious document, articulating a new service model with greater emphasis on primary and community care; increased emphasis on mental healthcare, prevention and health inequalities; a clear focus on quality and outcome improvement in areas where greater progress is seen as necessary; some workforce reforms; wholesale rebalancing of the NHS relationship with digital services and significant changes to the financial regime. The plan will be achieved by:
- Doing things differently. Giving people more control over their own health and the care they receive, encourage more collaboration between GPs, their teams and community services, as primary care network, to increase the services they can provide jointly. Increasing the focus on NHS organisations working with their local partners, as integrated care systems, to plan and deliver services, which meet the needs of their communities.
- Preventing illness and tackling health inequalities. The NHS will increase its contribution to tackling some of the most significant causes of ill health, acting to help people stop smoking, overcome drinking problems and avoid Type 2 diabetes, with a particular focus on the communities and groups of people most affected by these problems.
- Workforce. Increasing the NHS workforce, training and recruiting more professionals – including more clinical placements for undergraduate nurses, more medical school places, and more routes into the NHS such as apprenticeships.
- Making better use of data and digital technology. The NHS will provide more convenient access to services and health information for patients, with the new NHS app as a digital front door, better access to digital tools and patient records for staff, and improvements to the planning and delivery of services based on the analysis of patient and population data.
- Getting the most out of taxpayers’ investment in the NHS. Working with doctors and other health professionals to identify ways to reduce duplication in how clinical services are delivered, make better use of the NHS combined buying power to get commonly used products for cheaper, and reduce spend on administration.
Integrated Care Systems
The NHS Five Year Forward View published in 2014 established Sustainability and Transformation Partnerships (STPs). STPs are now evolving into Integrated Care Systems (ICSs). Within the current legal framework, the NHS and its partners will be moving to create Integrated Care Systems everywhere by April 2021, building on the progress already made. ICSs bring together local organisations in a pragmatic and practical way to deliver the triple integration of primary and specialist care, physical and mental health services, and health with social care. They will have a key role in working with Local Authorities at place level, and through ICSs, commissioners will make shared decisions with providers on population health, service redesign and long-term plan implementation. ICS will deliver the aims set out in the NHS long-term plan.
Could you present two/three elements on the impact of such reforms on hospital and/or healthcare sectors that your organisation/country has identified?
Vanguards
Following three years of testing alternative models in the Five Year Forward View through integrated care Vanguards and Integrated Care Systems, we now know enough to commit to a series of community service redesigns everywhere. The Vanguards received less than one tenth of 1% of NHS funding, but made a positive impact on emergency admissions, and demonstrated the benefits of proactively identifying, assessing and supporting patients at higher risk to help them stay independent for longer.
Moving care closer to people’s homes and communities
Frimley STP’s North East Hampshire and Farnham Vanguard brought together primary, community, acute, mental health and social care service teams across the area to work as one. Closer working across traditional service boundaries helped to stimulate new services and initiatives, which support people, to manage their own health and care more effectively and to receive more care and support in their local community rather than in hospitals.
This includes the Time Out café in Aldershot for people with mental health problems, run across geographical and organisational boundaries to offer an alternative to A&E for those in crisis. Service users can access the café seven days a week with no appointment needed, to get support from staff, learn self-management skills and use community resources such as peer support and mental health and wellbeing advice. The scheme has resulted in a reported 33% reduction in acute psychiatric admissions. Residents’ feedback shows they particularly value being able to access help when they need it and that the café has helped to avoid further crisis, self-harm and unnecessary A&E visits.
Other examples include GPs in Erewash are supporting urgent care through an on-day service that has contributed to a 3.8% fall in non-elective admissions to hospital, despite overall rising A&E attendances. In Dudley, teams of doctors, nurses and other professionals have reduced the time people spend in hospital by the equivalent of 900 bed days in just over two years. Pharmacists, working alongside teams in local GPs’ surgeries, have helped reduced mortality from hypertension.
Further case studies and examples can be found here.
References
1 For more information on the Danish National Strategy for Personalised Medicine 2017-2020 click here.
2 For more information about the National Digital Health Strategy 2018-2022 click here.
3 The reply was provided in January 2019. The reform mentioned did not receive the approval on the Finnish Parliament and the Government resigned in March 2019. Ministério da Saúde (2018), Retrato da Saúde, Portugal. Available here.
4 Portaria n.º 71/2018. Available here.
5 For further information click on the following link.
6 Ministério da Saúde (2018), Retrato da Saúde, Portugal. Available here.
7 Estratégia Nacional para o Ecossistema de Informação de Saúde 2020 (ENESIS 2020). Available here.
8 Web-portal available here.
9 Mobile application MySNS available here.
10 Mobile application MySNS TEMPOS available here.
11 Mobile application MySNS CARTEIRA available here.
12 Decreto-Lei n.º61/2018 available here.









